
Chronic Obstructive Pulmonary Disease is a group of illnesses affecting the respiratory system.
They cause decline in lung airflow and affect normal breathing. COPD is the third leading cause of death. However, with proper care, life expectancy for a patient in stage one and two can be decades.
The most effective way to ensure COPD does not increase the chances of early mortality is to follow all therapy guidelines. This is including but not restricted to smoking cessation and pulmonary rehabilitation.
Turn for the Worse
Exacerbation is an episode of symptom flare-up. It is characterized by worsening of symptoms like airway and systemic inflammation.
The cause of at least 70% of exacerbations is known, and in many cases, preventable. It may be anything from environmental factors to smoking.
The remaining 30% is attributed to different things, chief among them, pulmonary embolism.
This is only a matter of concern in severe flare ups. Severe flare ups demand hospitalization and clinical investigation.
With the prevalence of pulmonary embolism in COPD patients, it is becoming almost mandatory to run a battery of tests to determine the presence of PE.
Look into the Emboli
Pulmonary embolism is a blockage in the arteries in the lungs. These blockages are 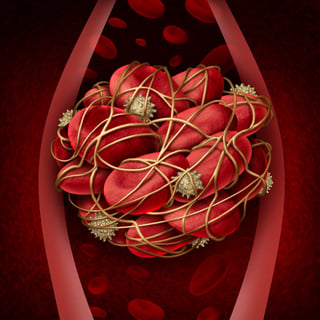 caused by blood clots.
caused by blood clots.
Most of the clots travel up from the lower extremities. In fact, up to 97% of pulmonary emboli originate from there. PE is a serious condition with a high mortality rate.
There are more than 180,000 new cases every year in the 45+ demographic.
The key to survival is early detection.
Post mortem studies show that 51% of COPD patients had pulmonary embolism. The three month mortality rate for COPD patients is 18%.
When PE is added to the mix, that percentage almost triples with a rate as high as 53%.
Diagnosing PE in COPD patients usually does not happen until it is too late. This is why most of the information about the PE prevalence comes from autopsy studies.
One should however look out for shortness of breath, chest pain, palpitations and coughing up blood.
It may look like a normal COPD flare up but it is best to see a doctor as a clot in the lung will kill quickly.
Root of the Problem
It is best to try and understand something before getting down to the brass tacks of getting rid of it.
There are a variety of causes that must be understood before prevention and a treatment plan can be hatched.
Blood clots are a defensive mechanism for the body. When an injury occurs, the body emits clotting agents to keep blood spillage to a minimum.
However, sometimes signals get mixed up and clots form inside the body. A clot is formed when platelets and plasma proteins thicken.
They form a gel like or semisolid substance. The effect of a small immobile clot is negligible. One is safe in this instance.
The problem comes in when the clot grows and disengages itself to travel through vessels.
There is no telling where it will end up. An arterial clot will cause immediate symptoms and is deadly. One will suffer severe pain, partial or full paralysis, heart attack and/or stroke.
Without emergency treatment, fatality is imminent. A venous clot will build up over time.
A special kind of venous clot causes DVT. In other words, Deep Vein Thrombosis. This is the development of clots in major veins; it is more common in the limbs.
1. Mobility
Movement aids blood circulation. If you remain largely sedentary, it hinders circulation  and puts you at greater risk for a blood clot.
and puts you at greater risk for a blood clot.
Sitting for long periods of time, causes blood to pool around the legs. After some time, the blood constituents start to combine and thicken.
These are the same clots that will travel up to the lungs and cause blockage.
COPD exacerbation demands that the patients stay in hospital for a few days depending on the degree.
They remain confined to the bed while treatment is being administered and samples are taken for investigation.
If the flare-up was too severe, the patient becomes semi-permanently immobile. The reduced mobility that comes with COPD conditions could very well be the reason a patient develops PE.
2. Vessel damage
Anything from injury to bruising during surgery can cause vessel wall damage. The vessel could also be damages by conditions such as varicose veins.
Treatment courses like chemotherapy are also harmful to the vessels.
If the wall of a vessel is damaged, the system will react as it would to a regular injury. The blood constituents will signal each other and band together to prevent spillage.
Even if this does not cause clotting, narrowing and blockage will cause the blood to pool.
COPD patients grow weaker by the day.
Fractures and other injuries become common when balance becomes a problem. They are also, sometimes, subjected to surgeries.
These are both conditions that could leave room for the vessel damage necessary for formation of clots.
3. Smoking
Smoking weakens the vessels. It makes the body work harder to pump blood therefore wearing out the vessels quite a bit.
Weak vessels are a recipe for clot formation.
The first thing a doctor instructs upon diagnosis of COPD is, quit smoking. Smoking is among the leading causes of COPD.
Smoking will shorten your lifespan and degrade your quality of life as your COPD worsens. When pulmonary embolism is thrown into the mix, it’s even more dangerous.
4. Age
Clots are prevalent in the over sixty demographic. This is because of their decreased activity.
People of this age group have been slowed down by the aging process. They walk slower and sit for longer periods of time.
They also spend more time on bed rest for age related illnesses. They are at a higher risk for developing clots.
The same demographic also suffers immensely under COPD.
It is usually under treated due to the presence of multiple comorbidities. This makes the elderly more prone to harboring both COPD and PE.
5. Additional Factors
Weight is an important factor in management of both pulmonary embolism and chronic obstructive pulmonary disease.
Body mass index is instrumental in keeping the forced vital capacity and forced expiratory volume in one second at optimum levels. The same encourages mobility.
Pulmonary emboli may be caused by small masses of infectious material or fat released after fractures or trauma.
Air bubbles or substances could also cause blockage therefore restricting blood and oxygen flow.
Cancerous tumors are also culprits of the same. Pulmonary embolism will cause COPD exacerbation, Tumors due to lung cancer could cause blockage of the pulmonary arteries.
When to Dial 911
Severe, on-going pain in any area of the body is a red flag. If the same area gets discolored within days and swelling occurs, try muscle pain relievers. If an ice pack does nothing, it may be time to see a doctor about it.
within days and swelling occurs, try muscle pain relievers. If an ice pack does nothing, it may be time to see a doctor about it.
There could also be instances of fainting due to low blood pressure.
The area should have a warm tingling sensation. It could be the first stages of clot formation.
If left to its own devices, the clot could grow to become very problematic.
For COPD patients, this is exactly the kind of problem to avoid.
If not attended to, it might go on to restrict free flow of oxygen in the lungs. Then an exacerbation looms.
Battery of Tests
When a doctor suspects pulmonary embolism in the event of a flare up and the patient is ripe for the risk factors, they will run a bunch of tests to confirm.
Some of these tests are only mildly invasive. The more rigorous ones are only ordered if the results lean towards positive results.
For example, if a CT- Scan shows possible signs of PE. A V/Q scan will be ordered.
This is a nuclear medicine scan that uses radiopharmaceuticals to examine pulmonary ventilation and perfusion.
The chief aim is to confirm presence of clots in the pulmonary arteries.
A pulmonary angiography is the use of dye to map out the vessels. Special instruments are then guided through the system in search of clots.
If DVT is suspected to be the beginning of emboli, other tests are carried out. A duplex venous ultrasound and venography provide detailed images of the venous structure in the legs.
It informs of the presence of more clots that could potentially lead to PE. D-dimer is another specialized blood test for the purpose of discovering clots.
Course of Treatment
Once PE has been confirmed to be a prevailing condition, the doctor may prescribe anti-coagulants to prevent new clots and dissolvers to break down existing ones.
The treatment plan is entirely up to the doctor as they know the patient best.
In some cases, surgery is called for.
The surgeon might install a vein filter in the vena cava. This is the vein that leads from the limbs to the lungs.
This is to prevent DVT clots from getting anywhere near the pulmonary veins. If they have already arrived, removal is necessary.
This is done by sucking out the clots using specialized implements. This procedure is risky but necessary at times.
What Can You Do?
As a patient, there are things to do to keep clots at bay. They are regular everyday activities but could be of significant advantage to the prevalence to pulmonary embolism as a COPD patient.
With increased age comes a greater likelihood of developing COPD pulmonary embolism.
This is not a factor that can be helped so it is best to concentrate on the things that can be changed, such is wisdom.
Obesity is one of these factors. Overweight and underweight are both equally bad. They have adverse effects on both COPD and PE.
Birth control pills have been said to increase the risk of clotting. In 2014, there was a study that proved non-steroidal anti-inflammatory drugs increased risk by as much as 80%.
These are common painkillers like ibuprofen. It was argued that the same painkillers contain anti-coagulants and are therefore harmless in that respect.
There was a lot of back and forth. The bottom line is, before using over the counter pain killers a COPD patient should consult their doctor for direction.
DVT is the most common cause of pulmonary emboli. Current and former patients should let their doctor know about this so that a screening can be done.
Early detection is key when it comes to COPD pulmonary embolism.
A family history of DVT or PE should be reported to the pulmonary specialist as a matter of urgency. This ensures the doctor stays on the lookout for symptoms of PE.
Keep Moving!
Even the least bit of activity could help. Movement aids blood flow. If you can't leave the house, even seated leg exercises can help.
This keeps blood from pooling in the legs therefore reducing risk of DVT. After a hospital procedure, try and get active as quickly as possible.
Even a walk up five steps is movement in the right direction. As long as body stays mobile, risk stays low.
Anti-inflammatory diet of omega 3, hydration and no smoking whatsoever. These are just simple lifestyle directions but whose effect is significant.
Consult your doctor before travel of any kind. If it is a long drive, frequent stop overs for stretching will help.
Be sure to stay hydrated to keep fluid from building up!
Compression stocking are also helpful in keeping DVT in check. They are worn at home to keep blood flowing for people who are at the highest risk for DVT.
The doctor must grant permission before these can be obtained.
Diabetes, ulcers, blood pressure and other lifestyle diseases should be kept at a safe distance.
Try to eat healthy and stay as active as possible!
This cannot be stressed enough, doctor should know about the possibility of genetic predisposition to any clotting disorders.
Managing COPD alone is an arduous task due to all the triggers in the air at all times. Keeping such vital information from the doctor almost guarantees adding another condition in need of management to the roster.
If detected early, pulmonary embolism can be managed and possibly eradicated completely. The key is to recognize the risks and symptoms so that action is prompt and effective.



